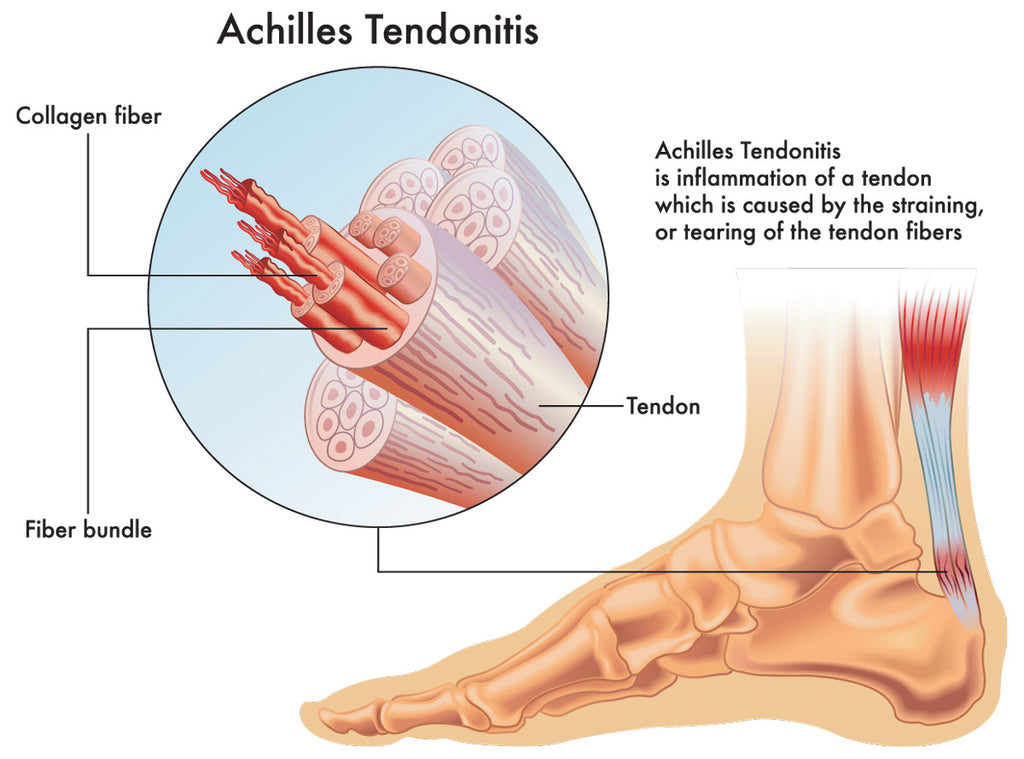
Achilles Tendonitis is a condition characterized by inflammation and irritation of the Achilles tendon, which is the thick band of tissue that connects the calf muscles to the heel bone. The Achilles tendon is the largest and strongest tendon in the body, named for the Greek god Achilles. It helps you walk, run and jump by raising the heel off the ground.
There are two types of Achilles tendinitis, which describe which part of the tendon is affected:
Noninsertional Achilles tendinitis wherein the fibers in the middle of the tendon start to break down, swell and thicken. This type of Achilles tendinitis affects people who are younger and more active.
Insertional Achilles tendinitis, which affects the lower part of the heel, where the tendon connects, or inserts, to the heel bone. It can affect anyone, even people who aren’t active. But it most commonly affects people who overuse the tendon, such as long-distance runners.
Who is at risk for Achilles tendonitis?
People at high risk for Achilles tendon disorders include those who:
- Play sports, especially sports that involve quick stops and starts or require jumping and quick changes of direction
- Run or dance
- Have jobs that put stress on their feet and ankles, such as laborers
- Participate in sports less frequently, i.e. “weekend warriors”, leaving their bodies less used to the stress
You may also be at higher risk for Achilles tendinitis because of your body shape and structure. For example, if you have:
- Tight or weak calf muscles
- Bone spur, an extra bone growth in your heel that rubs the tendon, causing pain
- Flat arches
- Overpronation, ankles that roll down and in when you walk
What are some common causes of Achilles tendonitis?
Although Achilles tendon disorders are common sports injuries, it can affect individuals of all ages who engage in activities that involve repetitive stress on the Achilles tendon, such as activities that require jumping and quick changes of direction. Some common causes include:
- Engaging in activities that require repetitive jumping, running, or sudden increases in intensity without adequate rest can strain the tendon.
- Wearing shoes that do not provide proper support or have inadequate cushioning can contribute to the development of Achilles tendonitis.
- Abnormal foot mechanics or gait abnormalities can place additional stress on the Achilles tendon.
- Tight calf muscles can increase tension on the Achilles tendon, increasing the risk of injury.
- Rapid changes in training intensity, such as suddenly increasing running distance or intensity, can strain the tendon.
How is Achilles tendonitis diagnosed?
Diagnosing Achilles tendonitis involves undergoing a physical exam. Your doctor will gently press on the affected area to determine the location of pain, tenderness or swelling. He or she will also evaluate the flexibility, alignment, range of motion and reflexes of your foot and ankle.
Your doctor may also order one or more of the following tests to assess your condition:
- X-rays. While X-rays can't visualize soft tissues such as tendons, they may help rule out other conditions that can cause similar symptoms.
- Ultrasound. This device uses sound waves to visualize soft tissues like tendons. Ultrasound can also produce real-time images of the Achilles tendon in motion, and color-Doppler ultrasound can evaluate blood flow around the tendon.
- Magnetic resonance imaging (MRI). Using radio waves and a very strong magnet, MRI machines can produce very detailed images of the Achilles tendon.

How is Achilles tendonitis treated?
The treatment of Achilles tendonitis aims to reduce pain, inflammation, and promote healing. vTreatment options include:
- Avoid activities that aggravate the condition. Resting the tendon allows it to heal.
- Applying ice to the affected area can help reduce inflammation and relieve pain.
- Put pressure on the tendon using athletic wrap or surgical tape.
- Elevate the foot so it’s above your heart to reduce swelling.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) may be recommended to reduce pain and inflammation.
- Specific exercises can help improve flexibility, strength, and stability of the calf muscles and Achilles tendon.
- Custom orthotics or footwear adjustments can provide proper support and reduce strain on the tendon.
- Eccentric Strengthening: This involves controlled lengthening of the calf muscles to help improve the strength of the Achilles tendon.
- Regular stretching of the calf muscles can help alleviate tension on the Achilles tendon.
- Bracing or Taping: These can provide additional support to the tendon during activities.
- Splint at night to help the Achilles tendon stay stretched while you sleep.
- Wear a walking boot or walking cast if the pain is severe.
- Corticosteroid Injections: In some cases, a healthcare provider might administer corticosteroid injections to reduce inflammation and pain. However, these are typically used cautiously due to potential side effects and the risk of tendon weakening.
- Shockwave therapy, which uses strong sound waves to reduce pain and promote healing.
What is brisement?
Brisement is a treatment option only in earlier stages of Achilles tendinitis, before it progresses to Achilles tendinosis. Providers inject anesthetic into the space around the tendon to break up scar tissue. You may need to have this procedure a few times.
When is surgery necessary?
If you’ve tried nonsurgical methods for six months and you’re still in pain, surgery might be considered for cases of chronic Achilles tendonitis or if the tendon has developed tears. A foot and ankle surgeon can suggest options based on your injury, age, preferences and activity level.
Surgical options include:
- Gastrocnemius recession: The surgeon lengthens the calf (gastrocnemius) muscles.
- Debridement and repair: If most of the tendon is healthy, the surgeon removes just the damaged part and stitches together the remaining healthy tendon. After the procedure, you’ll wear a boot or cast for a few weeks.
- Debridement with tendon transfer: If more than half of the Achilles tendon is damaged, then there’s not enough healthy part of the Achilles tendon to function. You need an Achilles tendon transfer. Your surgeon takes the tendon that helps the big toe point down and moves it to the heel bone. Treatment gives the damaged tendon enough strength to function. You’ll still be able to move your big toe, walk and even run. But you may not be able to play sports competitively after this procedure.
- Hydrocision TenJet®: This minimally invasive, ultrasound guided technique uses high velocity saline to break up scar tissue in the tendon. The pressurized saline acts as blade to selectively remove unhealthy tissue. This is done on an outpatient basis.
How painful is recovery from Achilles tendon surgery?
Some people still experience pain after surgery and one complication of surgery is a wound infection, which can be difficult to treat due to the location of the Achilles tendon. Most people have good results from Achilles tendinitis surgery, but the main factor that affects recovery is how much of the tendon was damaged. People with a lot of tendon damage need a longer recovery period. Physical therapy also plays a big role in rehabilitation, either as a treatment method or as part of your recovery from surgery. It can help you regain your strength and function.
The outcome of Achilles tendonitis treatment varies depending on the severity of the condition, how promptly it's treated, and how well the individual adheres to the recommended treatment plan. Most cases of Achilles tendonitis improve with conservative treatments; and individuals can expect to resume normal activities gradually as the tendon heals. However, recovery can take several weeks to months, especially in more severe cases. It's important to follow the healthcare provider's advice and engage in appropriate rehabilitation to prevent recurrence and promote a positive outcome.
Are there ways to prevent Achilles tendonitis?
To prevent Achilles tendonitis and reduce the risk of developing this condition, you can consider the following measures:
- Wear shoes that provide appropriate support and cushioning for your activities. Choose footwear with a good arch support and shock absorption to reduce strain on the Achilles tendon.
- Gradually increase the intensity, duration, and frequency of your physical activities. Avoid sudden spikes in activity that can overload the tendon.
- Always start your workouts with a proper warm-up that includes dynamic stretches to prepare your muscles and tendons for activity. Similarly, end your workouts with a cool-down routine that includes static stretches.
- Regularly stretch your calf muscles and Achilles tendon. Focus on gentle and gradual stretches to maintain flexibility.

- Incorporate calf-strengthening exercises into your routine to build strength and stability around the Achilles tendon.
- Engage in a variety of physical activities to avoid overloading a single muscle group or tendon. Cross-training can help reduce the risk of repetitive stress injuries.
- Pay attention to your running or exercise technique. Avoid excessive heel striking or overpronation, which can contribute to Achilles tendon strain.
- Allow adequate time for rest and recovery between workouts. Overtraining without sufficient recovery can increase the risk of injury.
- Address any biomechanical issues or gait abnormalities that might be contributing to increased stress on the Achilles tendon. Custom orthotics or inserts can help correct these issues.
- If you start to feel discomfort or pain in the Achilles tendon, reduce your activity level and allow time for recovery. Ignoring early signs of strain can lead to more serious injuries.
- Excess body weight can increase the load on the Achilles tendon. Maintaining a healthy weight can reduce the strain on your tendons and joints.
- Stay hydrated and maintain a balanced diet rich in nutrients that support tendon health, such as foods high in vitamins C and E.
- Keep your feet clean and dry to prevent skin irritation and potential issues that could affect your gait.
Remember that each person's body is different, so it's important to tailor your preventive strategies to your own needs and circumstances. If you're new to exercise or have a history of injuries, consider consulting with a healthcare professional or a physical therapist to develop a safe and effective exercise plan.
If you suspect you have Achilles tendonitis it’s important to see a healthcare provider immediately to assess the type and extent of damage, and to devise a treatment plan for your particular situation. Call your provider or go to an urgent care center if you have symptoms that don’t improve after a few weeks, severe pain, or signs of a ruptured tendon (including if you heard a popping sound).