Do you have a steady ache right at the back of the heel? Does it tend to get worse when walking or even just with a light touch? Does the pain ramps up when you're moving around or wearing tight shoes?If so you may have Heel Bursitis. If you do and if you've been resting or just woke up, those first steps can be a real pain. Some compare it to the sensation of something gritty in their shoe, but it's actually the heel causing the discomfort. It can make regular daily tasks a bit of a challenge.
What is heel bursitis?
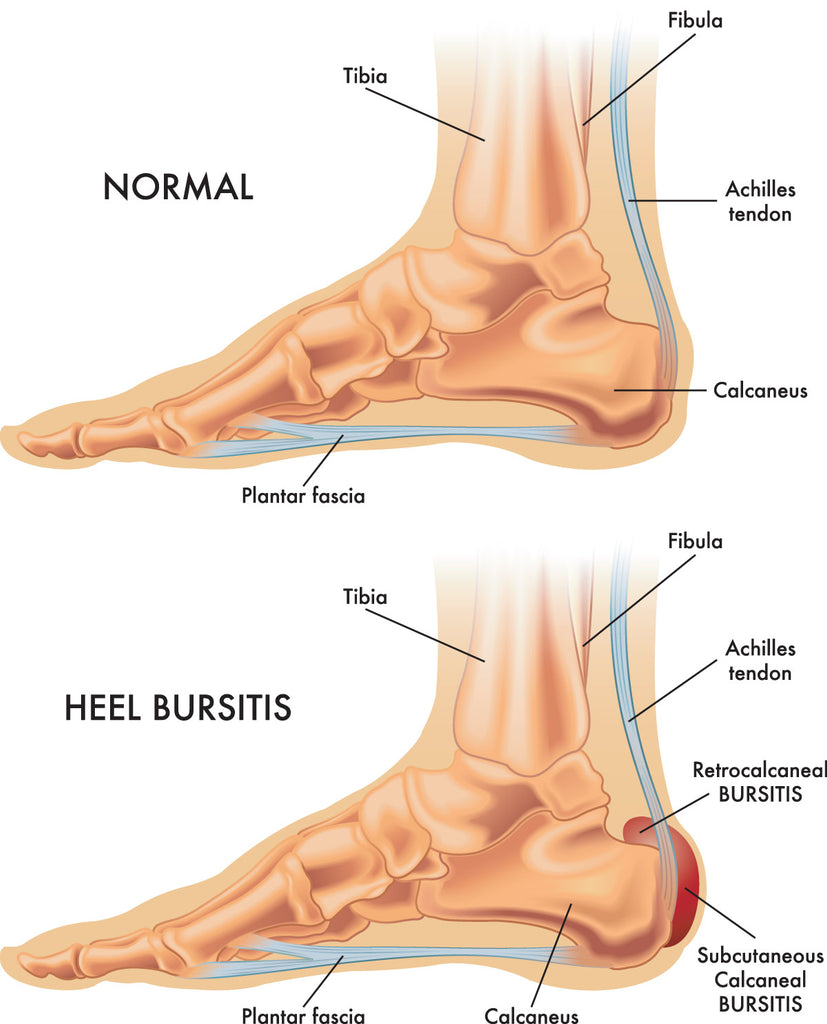
Heel bursitis, also known as Retrocalcaneal Bursitis, is a condition characterized by inflammation of the bursa located at the back of the heel where the Achilles tendon attaches to the calcaneus (heel bone). The bursa is a small fluid-filled sac that acts as a cushion between tendons, muscles, and bones, reducing friction and allowing smooth movement. When the bursae become irritated or inflamed it can result in heel pain, tenderness, swelling and ankle stiffness, known as bursitis. It is indicative of repeated overuse and injury to your heel. Some common causes include:
- Wearing the wrong shoes for the activity in which you are participating
- Repetitive activities that put strain on the heel, such as running, jumping, or wearing ill-fitting shoes
- Tight or inadequate footwear that puts pressure on the back of the heel
- Abnormal foot mechanics, such as flat feet or high arches, that can lead to improper distribution of weight and strain on the heel area
- Direct trauma or injury to the heel, which can cause inflammation of the bursa
What are the common symptoms of heel bursitis?
The main symptoms of heel bursitis include pain and tenderness at the back of the heel, particularly when pressure is applied or when walking, running, or standing for extended periods.
How is heel bursitis diagnosed?
To diagnose heel bursitis, a healthcare provider will typically perform a physical examination of the affected heel and ask about your medical history and recent activities. Imaging tests such as X-rays or ultrasound may be used to rule out other potential causes of heel pain and to assess the extent of inflammation and any structural abnormalities.
What treatment options are available?
The treatment for heel bursitis aims to relieve pain, reduce inflammation, and address the underlying causes. Common treatment approaches include:
- Rest: Avoiding activities that exacerbate the pain to allow the inflamed bursa to heal.
- Ice: Applying ice packs to the affected area to help reduce inflammation and alleviate pain.
- Footwear: Wearing properly fitting shoes with adequate cushioning and arch support can help alleviate pressure on the heel.
- Orthotic inserts: Customized shoe inserts can help correct foot mechanics and reduce strain on the bursa.
- Medications: Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce pain and inflammation.
- Physical therapy: Stretching and strengthening exercises can help improve foot mechanics and reduce strain on the heel area.
- Corticosteroid injections: In some cases, a healthcare provider may administer corticosteroid injections directly into the inflamed bursa to reduce inflammation and pain.
- Heel lifts: Elevating the heel slightly with heel lifts or pads can reduce pressure on the bursa.
With proper treatment and adherence to recommended lifestyle changes, the majority of cases of heel bursitis can be effectively managed. However, the outcome depends on the severity of the condition, the underlying causes, and the individual's response to treatment. In some cases, chronic inflammation or recurrent flare-ups may require more extensive interventions, such as advanced physical therapy or, in rare cases, surgical removal of the bursa.
Are there ways to prevent heel bursitis?
Preventing heel bursitis involves adopting healthy habits and practices that reduce the risk of developing inflammation in the bursa at the back of the heel. Here are some preventive measures:
- Choose Proper Footwear: Wear well-fitting shoes that provide adequate cushioning and support for your feet. Avoid shoes with excessive wear or those that don't provide proper arch support.
- Gradual Activity Increase: If you're engaging in activities that involve repetitive stress on the feet, such as running or jumping, make sure to gradually increase your intensity and duration. Sudden increases in activity can strain the heel area.
- Warm-Up and Stretching: Before engaging in physical activities, perform a proper warm-up routine and stretch your calf muscles and Achilles tendon. This can help prepare your muscles and reduce strain on the heel.
- Foot Mechanics: Pay attention to your foot mechanics. If you have flat feet, high arches, or other structural issues, consider using orthotic inserts or custom-made shoe inserts to improve foot alignment and reduce strain.
- Appropriate Shoes for Activities: Choose shoes that are specifically designed for the type of activity you're engaging in. Different sports and activities require different types of footwear to provide the right support and cushioning.
- Maintain a Healthy Weight: Excess weight can put additional strain on your feet and heels. Maintaining a healthy weight through proper diet and regular exercise can reduce the risk of heel bursitis.
- Rest and Recovery: Allow your body sufficient time to rest and recover after engaging in activities that put stress on your feet. Rest is crucial for preventing overuse injuries like bursitis.
- Avoid Hard Surfaces: Whenever possible, choose softer surfaces for exercise and activities, as hard surfaces can increase the impact on your feet and heels.
- Proper Technique: If you're participating in sports or exercises that involve jumping, running, or sudden movements, ensure you're using proper technique to minimize the strain on your feet.
- Listen to Your Body: Pay attention to any signs of discomfort or pain in your heel area. If you experience persistent pain, stop the activity and allow your body to recover.
- Regular Foot Care: Keep your feet clean and dry, and inspect them regularly for any signs of irritation, blisters, or other issues that could lead to heel bursitis.
If you have a history of foot problems or are experiencing chronic foot pain, consider consulting a podiatrist or orthopedic specialist. They can provide personalized advice and recommendations to prevent potential issues. By incorporating these preventive measures into your lifestyle, you can significantly reduce the risk of developing heel bursitis and other foot-related problems.
If you suspect you might have heel bursitis, it's important to consult a healthcare professional for an accurate diagnosis and appropriate treatment plan tailored to your specific situation.